Introduction
The pediatric population is particularly vulnerable to injuries of the anterior cruciate ligament (ACL), due to the intrinsic characteristics of such individuals. In effect, these are very active subjects; their tissues are still immature (greater joint laxity(1) and less strength); they experience a lesser sensation of danger in the face of risk situations; and they are moreover less adherent to treatment.
An increase in injuries of the ACL has been observed among pediatric patients in recent years, representing 26-65% of all cases of hemarthrosis in the youngest athletes(2). This increase (up to 2.3% annually in the last 20 years)(3) is mainly related to the growing number of children involved in high competition pivoting sports, and to early sports specialization(4).
The management of ACL lesions in pediatric patients has been very controversial. Many surgeons are concerned about the possible growth alterations following reconstruction of the ACL, secondary to physeal damage caused by the surgical approach, tunnel drilling or the plasty fixation systems used(5). However, delaying surgery is associated to increased meniscal and chondral lesions(6).
Furthermore, the skeletally immature knee possesses anatomic characteristics that distinguish it from the adult knee - particularly the presence of physes and the size of the intercondylar notch. It is therefore essential to know the maturity status when treating ACL lesions in these patients.
The present review seeks to contribute to better understand lesions of this kind in younger patients, facilitate decision making and unify concepts and strategies.
Diagnosis
Epidemiology and anamnesis
The knee in children is subjected to high pivot and contact demands not strictly related to sports activities. Nevertheless, sports is the most frequent cause of ACL injury in children(7).
In the case of knee pain following trauma in a child, we first need to compile a detailed case history, seeking to identify the causal mechanism. The anamnesis and physical examination are usually influenced by the emotional stress of the patient, which can condition the initial diagnosis(8).
The gender of the patient is very important, since girls have greater laxity(1) and a greater risk of ACL rupture(4,9) and associated lesions(10), and more difficulty returning to sports activity(11).
Age is also crucial in relation to decision making, with lesser joint maturity (increased laxity)(1) and bone maturity being associated to a greater risk of growth disorders due to physeal damage. The peak incidence of ACL injuries is between 15-18 years of age, while the highest revision surgery rates are found in patients approximately 14 years of age(12). Sexual maturity (based on the Tanner classification)(13), the puberty growth spurt or the comparison of body height versus siblings and parents are determinant factors in choosing the treatment for these injuries.
Childhood obesity, which in Spain reaches an incidence of 40%(14), also favours ACL injuries(15) and an increase in associated lesions(16).
The time elapsed from injury to surgery is decisive, particularly in relation to the associated lesions: delaying surgery more than 12 weeks from the time of the accident increases the incidence of meniscal and chondral lesions(6,10). This delay has been associated not only to the making of decisions on the part of the supervising surgeon but also to the socioeconomic situation of the patients(17,18,19).
The most common mechanism of injury in young patients is valgus and external rotation in the context of indirect trauma to the knee during sports activity(20). The patient usually presents pain, swelling and instability sensation with certain movements of the knee. Having reached this point, it is important to distinguish between acute and chronic lesions, since pain and inflammation predominate in the former, and instability sensation in the latter.
Physical examination
The patellar tap test evidences the existence of hemarthrosis. However, in children under 12 years of age this association is not so important, since the appearance of isolated meniscal lesions is equally likely as the appearance of ACL injuries (47%) - in contrast to patients between 12-18 years of age, where this association is observed in 65% of the cases of ACL injury(21).
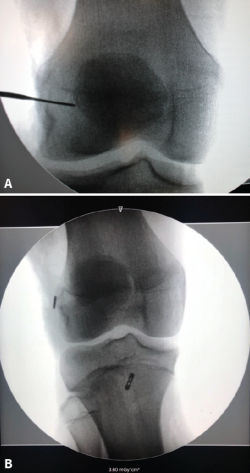
The specific tests used to explore ACL lesions in skeletally immature patients are no different from those used in adults. In this regard, the main tests are the Lachman test and the pivot shift test. The sensitivity of these tests may decrease due to the initial pain and limitation of joint balance. The exploration should be repeated after 2-3 weeks, once the pain and inflammation have subsided, and after full recovery of joint balance. In addition, this always should be repeated under anesthesia in the case of surgery, which is when the sensitivity of the physical examination is maximum: the sensitivity of the pivot shift test can increase from 35% in the consulting room to 98% under anesthesia(21). In acute lesions, the lever sign or Lelli test (Figure 1) has demonstrated greater sensitivity than the aforementioned tests(22).
[[{"fid":"4698","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"1":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
In addition to the diagnosis of the ACL lesion, we also must search for possible concomitant lesions: we should include meniscal provocation testing and also palpate both femoral condyles to discard possible osteochondral damage and assess competence of the extensor apparatus.
A lesion that is closely associated to damage to the ACL is the so-called lesion of the meniscal ramp of the posterior horn of the medial meniscus (though it has been little studied in skeletally immature patients). These lesions appear in about 25% of all cases(23) in the pediatric population with ACL injuries. A posteromedial port is crucial for establishing a correct diagnosis(23). Finochietto's sign (in the consulting room, under anesthesia and with arthroscopy) can contribute to the diagnosis of these lesions(24).
The knee in children is a much laxer joint than in the adult, and this should not be regarded as pathological. In all patients, regardless of their age, we must evaluate both knees in order to identify instability and not confuse it with hyperlaxity. In the case of pediatric patients this is even more important, however, since such laxity in these individuals is usually symmetrical, with no associated signs(1,25).
Complementary tests
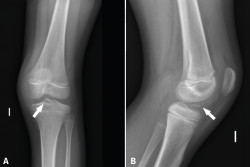
Plain radiographs (Rx)
Although the findings are usually normal, plain radiographs can help discard other types of lesions. Tibial spine fracture (Figure 2) in children can occur with a clinical history and physical examination findings similar to those of ACL injuries(26). In addition, radiographs allow us to assess other lesions (epiphysiolysis, fracture-avulsion of the inferior pole of the patella or fractures of the tibial tuberosity) characteristic of pediatric patients(27). Therefore, anteroposterior under loading and lateral Rx views of both knees are needed in the case of suspected ACL injury.
[[{"fid":"4699","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"2":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"2"}}]]
In pediatric patients, Rx studies are essential to establish true skeletal maturity. The most widely used methods include Rx of the knee(28), of the hand(29,30) or of the pelvis, according to ossification of the iliac crest (Risser classification)(31), or elbow.
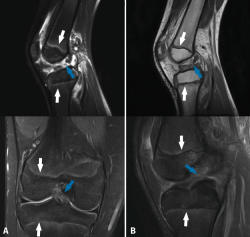
Magnetic resonance imaging (MRI)
Magnetic resonance imaging shows the physes in great detail in both the distal femur and in the proximal tibia (Figure 3), and is the best technique for evaluating them(30). The presence of the physes can complicate the diagnosis of ligament lesions in immature patients(32).
Magnetic resonance imaging allows precise assessment of the physeal condition of the patient(33). Physeal closure is directly proportional to age, though there are differences according to gender(28). Physeal closure is 0% until 11 years of age, 5% at 12 years, 34% at 13 years, 53% at 14 years, 94% at 15 years, and 100% from age 16 (33): this means that growth is complete in girls at about 14 years of age and in boys at approximately 16 years of age. Furthermore, the central portion of the physis of the proximal tibia closes before the peripheral portion - this fact being important for positioning of the tibial tunnel in ACL reconstruction.
[[{"fid":"4700","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"3":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"3"}}]]
Magnetic resonance imaging is also useful for the diagnosis of less frequent disorders such as agenesis of the cruciate ligaments (2/100,000 children)(34) - a condition that is usually asymptomatic and is associated to other anomalies around the knee(35) that can contribute to its identification.
Ultrasound
Although there are authors who defend its usefulness(36,37), ultrasound has not been standardized as a diagnostic tool in ACL lesions, and no data are yet available in skeletally immature patients. Nevertheless, the development of this technique in our specialty and its performance in the diagnosis of lesions associated to ACL injuries(38) suggest that ultrasound will grow in importance in the near future.
Treatment
Treatment decisions in the case of a pediatric patient with ACL rupture should be made by consensus among the physician, the patient and the parents or guardians.
The objectives of treatment are to:
- Restore normal knee function and stability, allowing an active and healthy lifestyle.
- Reduce the existing impact or risk of impact of meniscal or chondral disease, and the possible degenerative changes, as well as the need for future surgeries.
- Minimize the risk of arrested growth and/or deformity of the femur or tibia.
There are four fundamental aspects in the treatment of lesions of the ACL: prevention, conservative management and - in reference to surgical treatment - repair and reconstruction.
Prevention
Prevention is a crucial part of management, given the deleterious consequences of such disorders in this particular age group. Prevention programs seek to reduce the number of patients that may suffer a first ACL rupture, and to reduce recurrent rupture in those who resume sports activities after injury; these programs are able to avoid up to 53% of all ACL lesions, with increased evidence of efficacy in the case of plyometric, strength and agility exercises(39).
Perhaps the most popular of these protocols is the 11 + Kids(40), endorsed by the Fédération Internationale de Football Association (FIFA), and which has been shown to be able to reduce injuries(41) and is cost-effective(42). Another resource for the prevention of sports injuries is the Skadefri(43), a webpage developed by the Oslo Sports Trauma Research Center; it encompasses a broad range of sports and comes with a mobile phone application (Get Set) that can be very useful for injured patients.
Although there is evidence of the capacity of these prevention programs to avoid injuries(39), much work remains to be done - particularly on the part of the sports clubs and coaches(44). The main barriers for implementing these programs were found to be a lack of motivation, the technical requirements of the coaches and the needs referred to time during training, follow-up and cost(45) - though the same study proposed measures that should be introduced promptly, since prevention programs have been shown to be more effective when introduced at earlier ages(46).
Conservative management
Historically, ACL injuries in children have been subjected to conservative management (physiotherapy, orthoses and restriction of activities) until close to skeletal maturity, when ACL reconstruction was performed using techniques described in adults(47,48,49). Delaying surgery avoids iatrogenic alteration of the physis and allows the patient to reach the psychological maturity necessary to comply with postoperative therapy(50).
However, more recent studies have reported poor and unacceptable outcomes with conservative management: recurrent instability persists that favours meniscal and chondral damage, early degenerative changes and high sports dropout rates(10). Ramski et al.(51) found that patients treated on a conservative basis had a 33.7-fold higher probability of suffering clinical instability, and a 12-fold higher risk of developing medial meniscus rupture. The probability of returning to sports activity was 91.2-fold greater in the group subjected to early ACL reconstruction. The possible factors contributing to these poor outcomes include both the significantly higher activity levels seen in the pediatric population and patient failure to adhere to the modifications in the level of activity after the injury(47,48).
Conservative management could be a reasonable option in partial lesions of the ACL in patients under 14 years of age with tears affecting only the anteromedial fascicle, and with low Lachman test and pivot shift scores at exploration(52). In addition, the patients would have to comply with significant or total activity restriction, with the understanding that recurrent symptoms of instability might inevitably require ACL reconstruction surgery(53).
Conservative management is not recommended in patients with clear functional instability or subjects with concomitant intraarticular lesions requiring surgical treatment(54).
It is essential to provide the child and parents with detailed information on the surgical and conservative treatment options, the risks and the benefits. Likewise, the sports aspirations of the patient must be taken into consideration when deciding one treatment or other(49).
Close and frequent monitoring of the child is required in the form of repeated MRI scans and clinical examinations until skeletal maturation, and we must remain alert to instability episodes and secondary intraarticular lesions that would constitute an indication for immediate surgery(55). In the study published by Kocher et al., 31% of the patients subjected to conservative management required surgical reconstruction due to persistent symptoms of instability during sports activity(52).
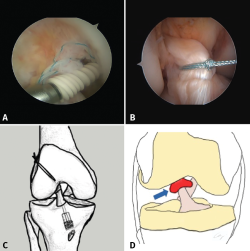
Repair of the anterior cruciate ligament in children: when, how and why
In recent years there has been renewed interest in the ACL repair techniques. This could afford some theoretical advantages with respect to reconstruction, such as preservation of the anatomy (insertion zone and morphology of the bands of the ACL, nerves and intrinsic cell population) and of some complex biomechanical properties of the ligament(56). In addition, recovery after such surgery seems to be faster and easier for the patient than following reconstruction(57).
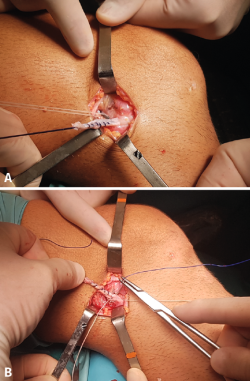
Primary repair is only indicated in patients with femoral avulsion of the ACL - Sherman(58) type I or, in some cases, type II; the proximal extremity of the ACL has better vascularization(59) and healing capacity(60) - and who preserve good quality tissue. This situation is usually found in the subacute phase (i.e., between 2 weeks and 3 months after injury) or in chronic ruptures if the ACL is adhered to the posterior cruciate ligament(61). Different techniques are available for ACL repair (Figure 4).
[[{"fid":"4701","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"4":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"4"}}]]
However, in the specific case of the pediatric population, the results are not fully conclusive: Gagliardi et al.(62) recorded a 10-fold higher probability of recurrent rupture and a cumulative three-year incidence of close to 50% in patients with repair versus patients with reconstruction, while Dabis et al.(63) observed no complications or failures over the short term (2 years) in 20 patients between 6-16 years of age subjected to direct repair surgery. The repair of ACL rupture in the pediatric population is an attractive option. However, based on the current state of development of the different techniques, it is not possible to establish a clear recommendation in favour of such surgery, and if this type of treatment is decided, the risks must be very carefully explained to the patient and family.
Reconstruction
Reconstruction is currently the treatment of choice in most pediatric cases. The different surgical techniques can be divided into two main groups according to whether they preserve the physes or not. In this section we will review the available techniques and different considerations regarding the choice of graft, the fixation systems, and the extraarticular plasties.
Techniques
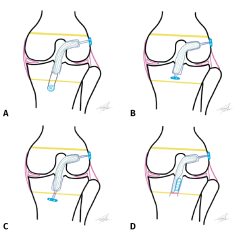
Techniques that avoid the physis
The physis lesion rates are much lower with these techniques, and the long term studies evidence few growth alterations(64). There are two subtypes of these techniques, according to whether bone tunnelling is performed or not:
• Epiphyseal techniques (all-epiphyseal procedures). Bone tunnels are made in the distal epiphysis of the femur and proximal epiphysis of the tibia, without perforating their respective physes. The first epiphyseal technique was described by Anderson(2) (Figure 5A), using quadruple ischiotibial autografts with bone tunnels made under radioscopic control. Femoral fixation is made with a suspension system, and tibial fixation is carried out knotting the plasty sutures to a screw anchored distal to the physis and medial to the tibial tuberosity. The modified technique of Cordasco-Green(65) (Figure 5B) uses a suspension system also for tibial fixation, in order to avoid the complications of the distal screw in the tibia or of an interference screw.
[[{"fid":"4702","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"5":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"5"}}]]
Wall(66) described a technique involving a double epiphyseal tunnel in the tibia and fixation in the femur with a screw. The double tibial tunnel allows the creation of a bone bridge (minimum 1 cm) that ensures tibial fixation without the need for an implant. Espejo-Reina et al. have likewise described a double tibial tunnel technique(67) (epiphyseal in the case of the proximal tunnel and diaphyseal in the case of the distal tunnel) to bridge the physis and avoid fixation systems in the epiphysis, due to the space limitations that are often found.
The epiphyseal techniques are not without a risk of damaging the physis. Early femoral physis closure rates of about 15% have been described(68,69). Wong et al.(70) concluded that any type of technique has its risk of physeal damage.
• Extraphyseal techniques. These techniques are carried out without bone tunnels. Micheli(71) and posteriorly Kocher(72) described the first technique destined for pediatric patients, using as plasty a portion of iliotibial (IT) band, preserving its distal insertion. By means of a combined extra- and intraarticular reconstruction, the portion of the IT band runs superficial to the lateral collateral ligament (LCL) towards an over-the-top position in the femur to enter the joint through the posterior intercondylar zone. Finally, after passing beneath the intermeniscal ligament, it is sutured in the periosteum of the anteromedial surface of the tibia.
Willimon(73) recorded a low reoperation rate with the technique of Micheli, without physeal alterations and with a return to the pre-lesion level of activity on the part of the patient. Kocher(74) recorded a satisfactory course in 240 knees, without growth alterations and with a low plasty rupture rate (6.6%). Nevertheless, this procedure also has disadvantages, such as the technical difficulty involved, the fact that it is a non-anatomic technique, and the production of lateral asymmetry at the IT band donor site in a large percentage of cases, without minimizing the high morbidity of the technique.
Techniques that perforate the growth physis (transphyseal techniques)
Tunnels are perforated in both physes (femur and tibia) in these techniques (Figure 5 C and D). These procedures are similar to those used in adults. The partial transphyseal technique is a hybrid procedure in which only one of the physes is tunnelled - normally the proximal tibial physis (Figure 6A). Since the tibial tunnel lies more perpendicular to the physis, the affected area is smaller, and the possible impact is considered to be minimal. Milewsky and Nissen(75) published their hybrid technique with good outcomes, though the patients presented dysmetria (1.2 and 2.2 cm). In a series of 24 patients, Chambers(76) reported four cases of physeal lesions and concluded that the procedure should be avoided in the youngest patients (Figure 6B).
[[{"fid":"4704","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"7":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"7"}}]]
Considerations regarding grafts in reconstruction of the anterior cruciate ligament in pediatric patients
The choice of graft is a key issue in all reconstructions of the ACL, especially in pediatric patients. Different options have been proposed, including ischiotibial plasty, IT band, patellar tendon, quadricipital tendon, allograft or parental donor tendons - each with its own particularities.
The plasty of choice is predetermined by the chosen surgical technique, and the latter in turn is conditioned by the age and bone maturity of the patient. Goosefoot tendon grafting is the most commonly used option, since there is great experience with its use, no bone blocks are left in the physis, and it facilitates the all-inside technique with two cortical suspension systems. The problem with this graft is that the thickness of the plasty is predetermined by the height and weight of the patient(77); in some cases the graft therefore may be too thin. Thus, the use of a quadricipital tendon graft without bone block has been proposed, with excellent results, similar to ischiotibial plasty(78). Nevertheless, a recent review of the national registry in New Zealand concluded that the thickness of both the ischiotibial plasty and of the patellar tendon does not affect the ACL plasty failure rate in young patients (under 20 years of age)(79). Some authors recommend supplementing the procedure with allografting and producing a hybrid graft of greater thickness(80) - though caution is required with this recommendation, since high recurrent rupture rates of these plasties in adult patients have been reported(81).
In skeletally immature patients we avoid the use of bone-patellar tendon-bone plasty, since the bone block may become interpositioned in the physis and cause epiphysiodesis.
In recent years, the use of parental live donor grafts has been proposed, offering the same benefits as allografting in terms of low morbidity, but with much fewer complications. These are ischiotibial grafts (only semitendinosus) of the parents in the same surgical step. This reduces the recurrent rupture rate, since it involves live tissue with the same mechanical properties; we avoid damage to the donor zone of the child; and the patient tendons are preserved for possible future revision surgery - in addition to ensuring adequate plasty thickness for the operation(82).
Plasty fixation systems
These systems depend on the technique employed and on the maturity status of the patient. It has been seen that femoral fixation with a suspensory button system does not differ significantly from fixation with an interference screw in relation to peak loading and cycles to failure(83). However, interference screws are not advised as fixation system in techniques that tunnel the physis, due to possible damage to the latter; they therefore should be contemplated in epiphyseal techniques. The suspensory button system is advised in techniques that tunnel the physis.
With regard to tibial fixation, suspensory fixation is recommended in the epiphyseal techniques or in partially transphyseal procedures. However, in advanced maturation stages we can use an interference screw as fixation system, due to the lesser incidence of growth anomalies involved - though it has been shown that there is an increase in local symptoms with this fixation system in one out of every 10 reconstructions of the ACL in young patients, with a 5% reoperation rate because of them(84).
Anterolateral extraarticular plasties
Isolated reconstruction of the ACL might not suffice to restore the knee to its pre-lesion state(85), and adding an extraarticular plasty to this operation provides better clinical outcomes with a decrease in recurrent rupture rate of up to 43%(86).
[[{"fid":"4705","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"8":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"8"}}]]
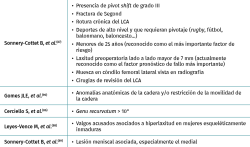
The main indications for combining a lateral extraarticular plasty were described by Sonnery-Cottet et al.(87); however, other indications have subsequently been incorporated(86,88,89,90) (Table 1). The main techniques for anterolateral reinforcement plasties may be non-anatomic (Arnold-Coker, modified Lemaire and Kocher-Micheli) or anatomic (reconstruction of the anterolateral ligament [ALL]):
• Arnold-Coker technique (modified MacIntosh). Use is made of an IT band plasty released proximally and left anchored distally. After passing it under the LCL, it is folded and sutured onto itself at the level of Gerdy's tubercle(91), avoiding the femoral tenoepiphysiodesis effect associated to the classical MacIntosh procedure(92) in children, with proximal fixation to the physis.
• Modified Lemaire technique. This is the most popular procedure, and a number of modifications have been developed. Use is made of an IT graft of sufficient length to allow it to be passed beneath the LCL for insertion in the femur, posterior and proximal to the epicondyle(93), though we must be very careful with the femoral physis. Some authors recommend positioning it in the femoral tunnel itself, under radioscopic control(88,90), thereby reducing the risk of physeal damage. Another modification involves suturing the plasty to the same femoral button as the ACL(88) (Figure 7).
• Kocher-Micheli technique. Already previously described among the extraphyseal techniques, this procedure combines reconstruction of the ACL with anterolateral reinforcement in the absence of bone tunnels. The objectives are to minimize the risk of physeal damage, facilitate revision surgery, preserve the traditional autografts and contribute an additional rotational stabilizer. The technique is an excellent option for the repair of ACL rupture in prepubertal athletes. The author considers the ideal patient profile to correspond to Tanner stage 1-2, boys < 12 years of age or girls < 11 years of age(72).
• Reconstruction of the ALL. The ALL has been anatomically described in pediatric subjects; its insertions have been shown to be in close relation to the femoral physes (10 mm distal on average) and tibial physes (9 mm on average)(94,95). Many techniques combine anatomic reconstruction of the ACL and ALL(96,97,98) in adults, not specifically in pediatric patients - though it has been shown that the indicated tunnels can be made safely(99). The lesser recurrent rupture rate and improved functional outcomes in adults(87,100), together with the high ACL plasty failure rates in skeletally immature patients(101,102), suggest that in the future the use of anterolateral reinforcements will increase in this population group.
[[{"fid":"4706","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"9":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"9"}}]]
Other technical considerations
Pediatric patients are characterized by a smaller intercondylar notch. However, routine intercondyloplasty (notchplasty) is not recommended in all patients, since it implies variation of the biomechanics of the knee (increased anterior translation of the tibia and reduction of plasty strength at low degrees of flexion) with at least 3 mm of resection(103).
On the other hand, the incidence of meniscal ramp lesions is similar to that seen in adults. Revision is therefore advised through the intercondylar notch in the posteromedial compartment, in view of its high incidence, with due repair if found, since it affects the biomechanics of ACL reconstructions(23).
Surgical treatment algorithm
In selecting the surgical technique, it is advisable to evaluate the skeletal and bone maturity of the patient. Pediatric patients amenable to ACL reconstruction surgery can be stratified according to the risk of growth alteration due to physis damage (Figure 8).
[[{"fid":"4707","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"10":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"10"}}]]
The main problem of ACL plasties in pediatric patients is not the alteration of the physes and the consequent growth discrepancies but the high recurrent rupture rate of the plasties. For this reason, the most important need is a correct surgical technique with adequate placement of the tunnels, and to repair the associated meniscal and chondral lesions, if possible, in order to improve the stability of the knee and combine an extraarticular plasty if considered necessary.
Figure 7 shows an interventional algorithm according to the maturity status of the patients. There is no current consensus regarding the surgical technique of choice. Excellent outcomes with an adequate return to sports activities and a low incidence of failures and physeal damage have been obtained with all-epiphyseal techniques in the youngest patients; however, there is a greater risk of limb overgrowth(104). Likewise, it has been demonstrated that the over-the-top technique also affords excellent results, though with a greater angular deformity rate(105).
Considering the above, it is advisable to individualize each case and assess the maturity status of the patient in order to optimize the surgical technique. The epiphyseal or partially transphyseal techniques are more similar to the ligament reconstructions in adults; the surgeon therefore may feel more comfortable working with these options. Most ACL ruptures in children occur in adolescents with less than one year from closure of the physis(12). This allows hybrid transphyseal reconstruction with a minimum risk of physeal damage. For this reason, and in view of its lesser technical difficulty, it is the most common option. Likewise, the current development of suspension systems and retrograde drill design, with the aid of intraoperative radioscopy, allow the minimization of bone and physeal damage with this surgery.
Postoperative protocol and rehabilitation
Rehabilitation must restore the dynamic stability of the knee(106); it should be exhaustive and individualized according to the physiological and psychological maturity of the child in order to secure good outcomes, and the parents or guardians must participate actively in daily rehabilitation(26). Specific adjustments will be needed according to the surgery carried out, the type of graft used, and the associated lesions.
The functional objectives must be modified and not copied from the protocols applicable to adults. Rehabilitation programs for children under 12 years of age(26) should make use of leisure exercises and variations in order to avoid boredom; isokinetic and jump tests on one leg (with caution); and the placement of greater emphasis on the quality of the movements than on the leg symmetry index. Rehabilitators with training and experience in this population group are required.
Use of orthoses and crutches
The effectiveness of orthoses in the postoperative period after ACL reconstruction is not known(107). Nevertheless, their use can be recommended during the prehabilitation phase and after surgery, during 2-6 weeks, until the objectives of the first phase have been reached - particularly in view of the usually poor adherence of such young patients to the strict care requirements. Orthoses can also be used to prevent hyperextension, control varus / valgus, enhance patient awareness, and provide protection against possible falls or impacts with other children. In patients subjected to ACL repair surgery, extension orthosis is maintained during two weeks(108).
With regard to the use of crutches, there are a number of recommendations, depending on the protocol used. The most widely accepted recommendations are:
• Isolated reconstruction of the ACL. Most guides advise assisted full loading during the first postoperative week, with progression conditioned to patient tolerance until full loading is reached after four weeks(109). In 1998, Tyler et al. concluded that there are no deleterious effects in relation to stability or function in initial assisted loading in isolated reconstructions of the ACL - anterior pain being less intense in this group due to greater stimulation of the vastus medialis muscle(110).
• Associated meniscus repair. There are two tendencies in this regard: the recommendation to avoid weight-bearing for 4-6 weeks on one hand, and the allowance of initial complete loading with the use of an extension immobilizer during the first 3-4 weeks on the other hand. In any case, flexion should be limited to 90º during the first 4-6 weeks. Articulated orthoses may be used for this purpose and, if early weight-bearing is allowed, it should be done in full extension.
Rehabilitation phases
Four postoperative rehabilitation phases(111) and a prehabilitation phase(112) have been established in the case of surgical treatment for ACL rupture (Table 2). In the two cases (i.e., operated upon or not), the reference of progression through the objectives is similar in both groups. However, there are different expectations in terms of progression and in the time to fully return to sports activities. In all cases we must be guided by clinical and functional objectives, and the return to sports activities will be conditioned to reaching these objectives(113).
[[{"fid":"4708","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"11":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"11"}}]]
In order to move from one phase to another we must reach the objectives established in each phase. The objective in the first phase is to achieve rapid functional recovery and important muscle activation. In phases 2 and 3, the objective is to ensure adequate alignment of the extremities, together with correct support and loading techniques. Finally, in phase 4, secondary prevention measures to avoid new injuries are established, and we seek to reach neuromuscular functional stability before the return to sports activity.
Return to sports activity
In patients not operated upon, the return to sports activity is estimated to take between 3-6 months, while in the case of surgical patients the minimum period is 9 months. Nevertheless, in the latter patients, it is advisable to wait for 10-12 months after surgery (in those individuals subjected to repair, a period of 5 months has been proposed(108), though the evidence is very limited). Following ACL reconstruction, the estimated percentage of patients that return to sports activity in the first 9 months is 50%, and this figure increases to 85% at one year after the operation(114). The return to activity is conditioned by the type of sports, and should be made on an individualized basis for each patient.
The risk of recurrent ACL rupture in those patients who return to high-risk activities (pivoting and jump sports) is greater in children, particularly during the first 12 months(115). Consequently, some authors even advise waiting for two years before returning to high-risk sports activities(101,116). Furthermore, the lack of adherence of these patients must be taken into account when contemplating the return to activity: concern about repeat injury and patient confidence in his or her injured knee have an impact upon the results after rehabilitation(26,117). Thus, it is advisable not to return to high intensity sports activity before 14 months, and the legal guardians should be informed about the increased risk of repeat rupture particularly in the first two years(117).
Once the child returns to sports, routine training should also incorporate an exhaustive program for the prevention of injuries similar to those described in the section on prevention(40,43).
A plasty rupture rate of over 20% has been estimated, together with a 14% incidence of rupture of the ACL of the contralateral knee(118). Rehabilitation is therefore an ideal moment for working the non-injured leg - this being important for reducing the risk of injury(119). The recurrent rupture rate reaches 23% during the first two years after surgery(120).
Conclusions
Damage to the ACL in skeletally immature patients is frequent and complicated to treat; this guide has therefore been developed to assist in pre-, intra- and postoperative decision making.
The surgeon must take the patient maturity status into account in order to select the appropriate surgical technique. The most recommended strategies are all-epiphyseal techniques or partially transphyseal procedures with cortical suspension systems and in some cases interference screws. Furthermore, the concomitant lesions must be treated and an extraarticular plasty should be added when necessary.
These injuries are associated to an increased incidence of recurrent rupture and potential added complications compared with the equivalent injuries in adults. An important part of our work therefore focuses on an adequate surgical technique, but particularly on correct postoperative rehabilitation and an adequate waiting period before returning to routine sports activity - especially in the context of higher levels of competition. Lastly, it is crucial to prevent future injuries through specialized programs for both the operated knee and for the contralateral knee, which is also exposed to an increased incidence of injury.